READERS SUMMARY:
1. HOW DOES OUR SPINE AFFECT OUR COLON?
2. CAN OUR BONY ALIGNMENT DICTATE DISEASE GENERATION?
3. IF BONES ARE OFF WHAT ELSE MIGHT BE OFF?
4. HOW DOES LEPTIN AND HORMONES TIE IN?
5. INTRODUCTION TO EPCOTx PROTOCOL AND THE MITOCHONDRIAL Rx.
Musical inspiration: Led Zeppelin “In through the Out door”
Today we are going to talk a bit about your “out door” as part of the brain gut series continues. Today I am going to show you how spinal biomechanics and defecation are intimately related to good or poor physiologic function and may result in illness. The human spine has 5 lumbar verterae and one block of bone distal to it called the sacrum. The sacrum forms the back bony wall of the pelvis. The pelvic skeleton is the anchor points for the pelvic muscles that support our pelvic and abdominal organs. One of these organs is our colon. Colon cancer is now the second most common cancer. In 1900 it was number 37th on the list of cancer deaths. What caused such a dramatic rise in 112 years? Could this some how be related to spinal degeneration and or the modern diet? How might some modern behaviors be additive to this puzzle?
The pelvis floor has many muscles in it but we are going to focus on the muscle group that connects the colon to the pelvis today to illustrate a point about how altered bio mechanics can lead to disease. The levator ani is a broad, thin muscle group, situated on the side of the pelvis. The levator ani is divided into three parts: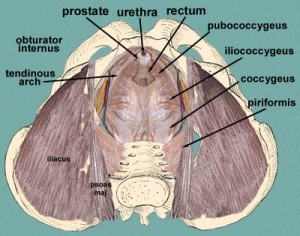
Iliococcygeus muscle
Pubococcygeus muscle
Puborectalis muscle
ANATOMY GEEK FEST: It is attached to the inner surface of the side of the lesser pelvis, and unites with its fellow of the opposite side to form the greater part of the floor of the pelvic cavity.
It supports the viscera in pelvic cavity, and surrounds the various structures which pass through it. The pelvic floor is different in men and women because their pelvic anatomy is quite different.
In combination with the coccygeus muscle, it forms the pelvic diaphragm.
The fibers which form a sling for the rectum are named the puborectalis or sphincter recti.
They arise from the lower part of the pubic symphysis, and from the superior fascia of the urogenital diaphragm.
NON GEEKS: These muscles act in unison normally to meet with the corresponding fibers of the opposite side around the lower part of the rectum, and form for it a strong sling. Relaxation of this sling increases the angle between rectum and anus, allowing defecation in conjunction with relaxation of the internal and external sphincters of the rectum. In essence, the muscles are designed by evolution to work best with the help of gravity. When we use gravity and the muscles together well we avoid disease of the colon. The combined action and coordination of these muscles allows us to avoid frequent bouts of colitis, hemorrhoids, constipation, inflammation of the proximal colon causing appendicitis, and possibly even colon cancer due to sustained chronic inflammation that can develop over time. This can also lead to many dysfunctions of pelvic floor if it is left untreated for decades.
COLON CANCER ALERT: 55{a7b724a0454d92c70890dedf5ec22a026af4df067c7b55aa6009b4d34d5da3c6} of colon cancers show up in the sigmoid colon and 25 {a7b724a0454d92c70890dedf5ec22a026af4df067c7b55aa6009b4d34d5da3c6} more show up in the cecum (proximal colon) where the appendix sits right behind the ileocecal valve. Remember that inflammation is usually present before cancer shows up. This may help you understand why appendicitis is so common today.
In my opinion, dysfunction of this valve due to inflammation is the most common cause of appendicitis in North America. The source of the inflammation can vary greatly. Heretofore, many people have looked predominately at the dietary causes of inflammation in the gut, but few people have thought how modern biomechanics of the spine might affect physiologic function of the colon. Today we are going to examine how your spinal biomechanics might be one of the major co variables in your colon issues.
GEEK FEST: The levator ani group relies heavily on the lumbo-sacral angle of the spine. This angle is formed by where the lumbar spine ends at L5 and the big bone of the sacrum (our vestige of a tail) is located in the pelvis. The greater the slip angle present in our spine, the more stress is placed upon the puborectalis muscle. This sling is altered when the spine loses it normal mobility or when we sit with our hips and knees at a 90 degree angle. This slip angle is increased by degenerative disc disease (DDD) of the L4-5 and L5-S1 discs or by a process called a spondylolisthesis. This problem can be inherited or can be acquired by a fracture in the pars interarticularis of the spinal vertebrae. It is not important that you know about these conditions unless you have been diagnosed with it already. When this process is chronic in the spine, it walks hand and hand with modic changes of the disc and vertebrae. This means the disc is dehydrated. Many people with modic changes also have dehydrated stools and this results in constipation. In my years as a spine surgeon I have noticed a correlation of severe colonic disease in my patients with DDD or in degenerative or lytic spinal slips. It became so clinically prominent in 2007, that I began to look for a link between the spinal angle and to colon disease. I found a relationship between the lumbo-sacral bony angle and anorectal angle.
NON GEEKS AND GEEKS UNITE: I found that patients with altered bony anatomy also had alter muscular anatomy and this lead to higher incidences of colon disease. Back then it did not seem like a great insight. Most spine surgeons know that bone position often dictates muscular action. What I failed to realize for ten years is how this alteration in biomechanics was tied to colon health. The link in the altered musculature of the proximal and distal colon due to this altered spinal and pelvic biomechanics. It appears as if the slip angle increases and the discs degeneration by losing water content while simultaneously these people lost the ability to hydrate their stools well because of the longer transit times in the colon. Many times these patients would require enemas and dis-impaction post op by our nursing staff after surgery on their spine. After I made this link I decided I needed to figure out a way to help offset this in these patients to help them. It was here I began toying with the idea of improving mitochondrial efficiency of their smooth muscles in theor colon’s to help inflammation and transit time. I came up with the Mitochondrial Rx and the EPCOTx plans. My members have already heard the webinar on the the EPCOTx protocol. Soon I will release the Mitochondrial Rx on the blog. I have found it has many more clinical uses than just helping the colon.
span style=”text-decoration: underline;”>MORE GEEKINESS?
What did I also find in almost all these patients clinically? The common tie in these patients was some degree of DDD, low iodine levels, disc dehydration, higher HS CRP’s, low DHEA and Vitamin D levels on their labs. Many also had altered testosterone and progesterone levels too. These things all made sense when I learned about the ties of sex steroid levels and gut flora. We covered that in Brain Gut 9, so maybe you hit the link and review it now. After three years of observation, I was convinced these findings had to be correlated with things also present in the colon directly. So on some of my patients I began to ask them to consider get formal GI testing with their doctors and using Metametrix GI testing. Some also had PCR analysis done of their gut flora when I explained the situation to them. Many told me of years complaining of constipation to their PCP and GI doctors and just got told to eat more fiber. That made their problems worse by report. Pro and prebiotics will help but they wont solve an altered gut flora and altered hormone panels.
The common ties I found were that most people with these spine problems had higher levels of inflammation systemically in their serum labs but it also correlated with alterations in their SCFA profiles and low butyrate levels in their colon. This connection had profound meaning to their clinical symptoms. Most also had altered gut flora’s as well by history and lab testing. I felt I might have stumbled into something important. When I tested them further, I often found very altered sex steroid levels and pretty significant hypothyroidism. Often times they were being treated for hypothyroidism with T4 only meds and they needed more support to help their colons and spines work better. Hypothyroidism is a sure sign of leptin resistance and the major underlying cause of mitochondrial dysfunction as you will see later this year on the blog. The patients who tended to be more obese with less mobility of their spines had more significant DDD and colon diseases.
This appeared to be another way the brain gut axis acted together in illness to cause disease in both organ systems. The larger the patient was (especially the belly) the higher the incidence and prevalence of constipation and hemorrhoids seemed to be. I also noted that the mobility of their spinal biomechanics was very abnormal in most cases. This did not surprise me as a spine surgeon but the link to colon disease was pretty remarkable consistent observation. Most of these patients insidiously lost the intrinsic ability to flex, extend and rotate their lumbar and sacral spines normally.
NON GEEKS: What does all that mean doc? It means when our spine has its normal ability to move gravity does most of the hard work of moving stool out of our colon. It also means transit time in our colon is dramatically reduced. Why is this important? Because the colon’s main goal is to reabsorb water and some electrolytes from our turds during transit to our rectum for elimination. If the turd sits in our colon too long, too much water is reabsorbed from it, and we go from a Bristol stool # 4 to a # 1, and this results in a hard stool that is difficult to pass. Suddenly one can see intuitively how diverticulitis, appendicitis and hemorrhoids would result in these patients. Moreover, we also see a simultaneous “upside down progesterone to estrogen ratio” and low levels of vitamin K2 and CoEnzyme Q10 when we test. This is how constipation has become enemy number one in people with DDD, spine disease and colon disorders.
This is also complicated by body mass and composition, which are both tied to hormone levels too. The size, shape and weight of the abdomen and chest is designed to push downward with gravity against our thighs which act as a buttress stabilizer of the squatting position. This position naturally compresses the colon to allow easy delivery of the turd without much effort from the walls of the colon. If one has to expend more energy to deliver the turd you get diverticulitis in the colon wall and or hemorrhoids at the exit of the GI tract. Said another way, when chronic effort is needed to expel a turd over decades due to loss of bowel water or poor smooth muscle function of the colon, colon disease like constipation, hemorrhoids, and inflammation are the result.
MECHANISM: ALL UNITE
When inflammation is chronic it can lead to a loss of cellular signaling and cause cancer formation to begin by altering the epigenetics of the p53 gene. This gene is the protector of our genome and works well when butyrate and inflammation levels are balanced. All these biomechanical actions are coordinated by the brain and guts innervation. Gentle pressure from the diaphragm supplements the force of gravity. The diaphragm is innervate by the C3,4,5 nerves. The levator ani is innervated by sacral nerves, and all the gut viscera down to the transverse mesocolon is innervated by cranial nerve ten the vagus nerve.
This implies that defecation is a very complex coordination of the central and peripheral nervous systems. This means if your brain is suboptimal in any way so may your ability to void well. Any breakdown in any area of this complex behavior will ultimately lead us to problems. Modern humans have a tremendous amount of spine disease and colonic illnesses for a reason. Even just the manner we sit on a toilet is a problem when one considers the bio mechanics. Consider this video from the folks at squatty potty!
Inflammation is most common in those eating a SAD, with low DHA and iodine levels and poor hydration. We cover this in some detail in the December 2012 Webinar if you want to learn more about the mechanism. This leads to an altered gut flora and alterations in the progesterone to estradiol levels which keep the gut flora from improving to an Optimal physiologic microbiome. Over time an altered gut flora changes the ability of the distal colon to handle SCFA and the production of buytrate. Over time lowered buytrate alters normal omega 3 levels in the distal and proximal colon and inflammation comes first and cancer follows it over time. Diverticulitis, appendicitis, constipation, gas, and hemorrhoids are warning signs of what is going on in your colon. Pay attention to these signs because they are all reversible.
What about the proximal valve in the colon doc?
The ileocecal valve, between the colon and the small intestine, has to be properly sealed to deliver a Bristol stool 4 consistently. The reason for this is simple. It creates the vacuum effect behind the turd to allow it to be propelled distally by allowing the proximal colon to be fully pressurized during digestion. This is often disturbed because of transit time increases and poor magnesium levels that weaken colonic mucosa. This is why diverticulitis is so common (80{a7b724a0454d92c70890dedf5ec22a026af4df067c7b55aa6009b4d34d5da3c6}) in people with spinal disorders.
Diverticulitis is a clinical sign of a weakened ileocecal valve. The proximal pressure in the colon also creates a natural laxative effect via propulsion. It acts like a turbo boost for stool transit. In the sitting position for humans the ileocecal valve is not well supported by the lumbo sacral spinal and pelvic ring and this bio mechanical weakness can cause the valve to become leaky to insufflation. This makes it difficult to generate the required proximal pressure to propel the stool out easily. When this occurs chronically diverticulitis and hemorrhoids predominate.
When spinal bio mechanics are improved with training or by squatting with defacation this action helps to support and relaxes the puborectalis muscle, which normally chokes and seals the distal rectum to maintain continence. When this is off humans also report they flatulate and pass gas often and quickly. People who tend to pass gas often have poor sleep efficiency and very low magnesium and CoEnzyme Q10 levels. They also have elevated HS CRP levels. These labs correlate amazingly well with degenerative spinal disorders. This is another clinical sign of mitochondrial dysfunction and inefficiency. This inefficiency is usually below 50{a7b724a0454d92c70890dedf5ec22a026af4df067c7b55aa6009b4d34d5da3c6} and it can even decrease the available bio-energentic substrates that need to be present for us to make ATP and use it in our mitochondria. We cover this in the webinar and in the future blog on the Mitochondrial Rx. If this situation occurs chronically, this can also lead to more serious colon disease like cancer.
Squatting during defecation elevates the sigmoid colon by 30-50 degrees to unlock the “hose kink” at the proximal rectum to allow easy delivery of the stool to eliminate it. This rectal bending by the muscle also helps prevent fecal incontinence, by taking some of the pressure off the puborectalis muscle. This is very common in older women (over 35) who have had many vaginal births. Women are more prone to this issue because of childbirth and differences in their lumbosacral slip angles than men to help them deliver live births. It is also why midwives like to use the semi squat position to deliver vaginal births easily. You would think people would see the homology in delivering a 7 pound child and a large stool from a biomechanical advantage but most do not.
SUMMARY:
Many of my patients with limited spinal mobility often raise their toilet seat heights because they can’t get their bottom low enough to reach the modern toilet. I tell them if they do that they must also get a stool to bend their knees and hips to improve the spinal biomechanics to help them eliminate their waste. If they do not listen they often develop hemorrhoids, diverticulitis flare ups, appendicitis, constipation, and bad gas. I have seen a few of my younger patients with different AI colon diseases also go one to develop serious cancers before the age of 35 too. The reason is AI’s have higher levels of inflammation by definition, so the disease shows up earlier in them that those without an AI. Modern medicine is perplexed by these cases because they have not thought about how we are intended to work by nature. Gravity is used by evolutionary design to help us deliver babies and waste. Keeping your spinal alignment and biomechanics optimal is quite helpful in these situations. If you have bad spine disease or any of these colon issues consider lowering your toilet height if your spine mobility can handle it, and if it can’t, then consider making yourself a stool for your feet to rest on while your eliminating yesterdays food. The goal is to get your knees and hips flexed enough against your torso to make your elimination quick and reliable. I like 30-40{a7b724a0454d92c70890dedf5ec22a026af4df067c7b55aa6009b4d34d5da3c6} of flexion in these cases.
If you want some modern convenience to solve this problem look into the squatty potty, and check out their video above. I want to leave with this thought that makes the point of looking for targets we do not yet see, but we know exist to help us reverse disease:
We have become so “smart” as a species that now we can even screw up our own biology for the sake of technology………Even the modern toilet can hamper us. Sitting does not equal squatting.
We need to connect the dots of illness and things we observe and do not have good answers for as yet.
When you know better you begin to do better………period.
CITES:
1. Wallner C, Maas C, Dabhoiwala N, Lamers W, Deruiter M (2006). “Evidence for the innervation of the puborectalis muscle by the levator ani nerve.”. Neurogastroenterol Motil 18 (12): 1121–2.
2. http://www.toilet-related-ailments.com/sikirov.html
3. http://www.ncbi.nlm.nih.gov/pubmed/447496?dopt=Abstract

