Readers Summary
- How might I correct a cortisol problem?
- How might I deal with a low cortisol?
- How might I deal with a high cortisol?
Cortisol is a glucocorticoid hormone. It is the most important one in humans, produced by the adrenal cortex and participates in the body’s homeostasis and stress responses. Cortisol concentrations also follow a circadian rhythm. It is a more complex rhythm than the human melatonin rhythm. Unlike the melatonin rhythm, human cortisol rhythms do not seem to be totally associated with day and night per se but seem to be more closely tied to the “transition periods” from dark to light and to a lesser extent, from light to dark. Transitioning light levels play a tremendous role in cortisol rhythms in humans. In addition to its circadian rhythm exhibiting a predictable peak in the morning, cortisol levels typically elevate sharply in the morning, 30 minutes to an hour after awakening. The glucocorticoid levels synthesized by the adrenal gland across the 24 hour day appear to be under the control of two distinct systems, one governed by the hypothalamic-pituitary-adrenal (HPA) axis, and one controlled by the autonomic nervous system through the adrenal medulla. Evidence supports that cortisol production can be uncoupled from the HPA axis controller of its release (ACTH). Night time light stimulates the suprachiasmatic nucleus (SCN) and this sends a neural signal to the autonomic systems to increase cortisol production from the adrenal gland, but not the brain. This can happen via the skin because of opsins present in the skin and fat. This is not coupled to pulsatile ACTH release in the pituitary (POMC) and has separate neural pathways. Studies have shown that exposure to high levels of polychromatic (white) light (80 lux at the cornea) in the morning, but not in the evening, could increase cortisol levels in humans. It appears the intensity of light and the route we get the light stimulus is critical to the real effect on cortisol levels. Studies have also shown that morning light can increase heart rate, suggesting an impact of light on the autonomic nervous system that modulates cortisol release from the adrenal gland. More recent studies have shown bright light to dramatically reduces cortisol levels in humans. (Second Cite)
Artificial light has a ton of blue and green light in destroying the cortisol/DHEA/Melatonin cycle. Low melatonin destroys mitochondrial autophagy. Red light seems safest based on what we know today.
Most of the readers of this blog should already understand that the most common cause of elevated cortisol in the USA is from obesity, so weight loss garners a lot of attention as a key treatment modality to lower cortisol levels. Today, we are going to talk about cortisol more in depth in how we managed it clinically.

What to do when cortisol is low like in adrenal fatigue
Many believe that one can solve lowered cortisol levels by just eating more carbs. This sounds great on the surface, but no one should be dogmatic about this without a proper biologic context. Lets talk about why this is the case. Cortisol production can best be enhanced by correcting most of the other hormone deficiencies that influence the biochemical pathways used by the adrenal glands first. Rarely is cortisol insufficiency a hormone problem in isolation. Cortisol is also a slow acting hormone as it effects the cell. It usually occurs with several other deficiencies present. These further complicate its diagnosis and treatment correctly in my view. The best way to repair the lowered cortisol deficit is to optimize hormonal function and allow the body to re adjust to circadian cycles. Often, patients symptoms become so severe that waiting for allostasis is clinically not an ideal choice.
The principal hormone replacement therapies that can increase the secretion of cortisol and/or its action are by increasing the anabolic steroid and sex steroids like testosterone, dihydrotestosterone, and estrogen. This is true in both men and women. These are both potent stimulators of reestablishing the normal diurnal cortisol production in humans. The reason is quite simple. When the more distal sex hormones are all in adequate supply, very little shunting of the substrate hormone, pregnenolone, is taken away from adrenal cortisol production pathway. The same is true of DHEA levels to a lesser degree. This is classically seen in a pregnenolone steal syndrome. Most people with adrenal fatigue suffer some sort of co-morbid hormone issue due to the central retinal pathways connection to the pituitary.
Many people ask me about the importance of thyroid hormone in this clinical scenario. Thyroid hormones are only mild stimulators of cortisol production pathways in humans. Much stronger biochemical inhibiters of cortisol production are high growth hormone levels (great body comp), hyperthyroidism (low TSH levels), and those with melatonin excess (exogenous supplementation). So people with high IGF-1 levels, low TSH levels, and those who sleep well, generally have low cortisol levels. Mild inhibitors to cortisol production are those women on oral estrogen. BCP’s make adrenal fatigue more likely, as does fludrocortisone, and those with elevated aldosterone levels. People with high aldosterone levels have higher blood pressures. They also have lowered thyroid hormones, lowered sex steroid hormones as well. People with low blood pressures have lower cortisol levels and lower aldosterone levels. When people have low cortisol production in the morning, and increasing cortisol levels at night, there are many ways to naturally boost the cortisol levels to balance the circadian cycle back to normal.
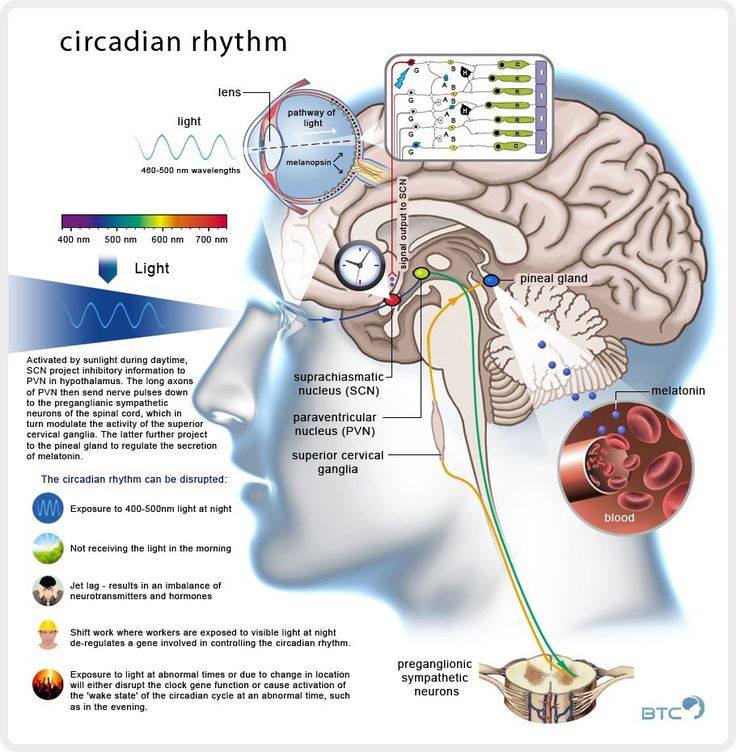
In the blogosphere, many default to recommend eating more carbohydrates to elevate cortisol in adrenal fatigue cases. They seem to think that the carbs are somehow the “magic bullet” for this condition. They are not the best choice in my view, but eating them will might help a person temporarily. Consumption of carbs will stimulate the ultradian cycle of cortisol production. This occurs because the presence of carbohydrates are associated with the longer light cycles seasons from an evolutionary timeline. Light in seasons has a power density relationship Light from the sun is the most effective way to alter your cortisol levels, because of its dramatic effects on the circadian cycle. If you don’t believe it, try eating carbohydrates in the winter for adrenal fatigue. This is usually an epic failure for patients clinically, because the light cycles are a stronger stimulus to an allostatic control of cortisol levels than carbohydrates are when the brain senses a short day via the eye. Why does this occur, you ask? Because sunlight or bright artificial light are potent effectors of the cortisol pathways via the retina and skin. The cortisol awakening response is highest at sunrise, due to a release of cortisol from the hippocampus in the brain. It is the hormone that wakes us up daily because it allows water to flow through our aquaporin gates. It is lowest at night when light ends. Bright light diminishes cortisol if the dose of light is high, while darkness seems to lower it as time increases in it. The cortisol awakening response is larger when people wake up in light rather than darkness. Therefore, light is the most effective means of controlling our cortisol production that we can use clinically.
Cortisol awakening response is increased in those who:
- waking up for a working day compared to the non working weekend day.
- experiencing chronic mental stress and emotional worry
- overloaded with tasks
- suffering the acute stress of any type via the PVN.
- are worn down by burnout (PTSD). Some studies find an increased though other researchers find a decreased or normal response.
Night time artificial light also raises cortisol levels, because our pineal-thyroid circuits have not evolved an off switch for artificial light as yet. Global control of gluconeogenesis is mediated by glucagon. Glucagon is released when our blood glucose is low and is unaffected by the light cycle. Glucagon generally is released from the human GI tract at night when we are sleeping to maintain our blood glucose while we sleep and not feeding.
Many patients report that a small amount of carbs help them sleep at bedtime. This is impossible if one’s liver is working correctly, because gluconeogenesis is turned off when glucose is present in our blood usually. When I hear this, I immediately know this person is compensating for another hormonal deficit. Only when we are in ketosis is gluconeogenesis stimulated! A small amount of dietary carbs should not be stimulatory to sleep, much less, the hepatic pathway of gluconeogenesis; low levels of carbs are instead required for it to occur. Glucagon augments ketosis further, and it is the failure of glucagon to act that actually promotes the adrenal pathways which might lead to adrenal fatigue if not enough carbs are eaten. In my experience, people with the highest risk of adrenal fatigue are generally those with blue light toxicity in the retina and results in poor hepatic gluconeogenesis, lowered dopamine production, and not from a lack of a dietary carbohydrates. One would be wise to adjust or tighten their light cycles first, then fix their liver problems next, before they consider eating a lot of carbohydrates to fix their adrenal fatigue first. Most people choose the carbohydrate pathway choice because it is most convenient in our current neolithic world. It is a horrible decision.There is nothing special biochemically about those people who are not at risk for adrenal fatigue. People most at risk for adrenal fatigue are those with poor gut/liver function, and they usually are LR or have low HDL’s on lab testing. I covered this in a previous blog here.
The principal lifestyle changes that you “might consider” strengthen the clinical effects of cortisol are as follows:
- Increase your exposure to sunlight, especially in the morning, and maximize darkness at night by sleeping with an eye mask at night and try to avoid all artificial light after dusk. New electronics put out unreal amounts of light, and completely destroy our normal circadian cortisol cycles more than any other behavior we engage in, including obesity. You must “tighten” your retinal exposure to sunlight, because this sharpens our brain’s perception of our circadian cycle of melatonin in the pineal-thyroid neural pathways in the brain. When you pay attention to the AM light cycle, it helps tremendously optimizing your appropriate diurnal cortisol levels during the day, and minimizes cortisol production at night. It is critical to avoid living and working in semi-darkness during the day. For example, a radiologist who works in a dark room looking at films all day is at big time risk for cortisol problems. People who work in mines during day break hours carry the same risk. People who work in semiconductor clean rooms under bright light at night carry the same risks as well. Following the light cycles for cortisol is a critical point that really should be followed strictly by all patients who are clinically trying to optimize their own cortisol levels daily. I also do not advocate wearing sunglasses in the daytime because of the circuit, no matter the season we are in. Humans tend to be very sensitive to loss of light in the winter months because of a lack of sunlight.
- At each meal, blood levels of cortisol normally temporarily triple regardless of macronutrients in the meal! Many people think that only dietary carbohydrates do this but this is not true. Dietary saturated fat (LDL levels/hydrogen) is necessary for the production of cortisol as saturated fat cholesterol is the first building block for cortisol synthesis. Carbohydrates do not form the building blocks of cortisol production at all. Our Epi-paleo template should aspire to avoid most alcohol, acids, caffeinated beverages, sugars and sweets, most soft drinks with fructose, most baked goods like bread, pastas and cereal grains. You should avoid all cereal fiber and all milk products, especially those with casein proteins to modulate cortisol levels. The blue light/nnEMF you allow the more salt you will need. An evolutionary blueprint is a great way to avoid these pitfalls.
- Beverages with caffeine (coffee, tea, cola) and alcohol should be avoided before bedtime as caffeine can increase cortisol (adenosine), and considerably reduce night-time secretion of melatonin from the pineal and retina. It also reduces serotonin from the gut used to help augment pineal melatonin production. Melatonin is a hormone that tends to reduce any cortisol production at night, improves mitochondrial function, and leads to autophagy/mitophagy. Remember that cortisol is supposed to be very low at night when melatonin is high. Sunlight in the AM lowers cortisol and adrenalin our blood. Melatonin production is increased in the retina and gut by a photochemical mediated pathway that converts serotonin to melatonin in the pineal gland after 4 hours of complete darkness. Dietary starches and sugars increase the blood sugar level, which in turn decreases gluconeogenesis, increases insulin, disturbs glucagon homeostasis, and reduces cortisol production. This is but another reason we might consider avoiding carbohydrates in the Leptin Rx reset protocol after dinner, on top of the insulin spikes that disrupt the leptin circadian cycle as well at night time. Carbohydrates out of season also deplete ATP compared to fats. They also decrease the amount of water produced in the matrix. Carbohydrates cause cells to swell through alteration of enzymatic kinetics due to proton issues. This slows the energy substrates that re-form ATP in our mitochondria. This slows our ability to replenish energy and decreases sleep efficiency at night. It also is clinically correlated with poor cortisol and DHEA levels.
- The excessive and prolonged stress of any kind exhausts the adrenal glands because of changes in the retina and brainstem at the paraventricular nucleus. Dopamine control of prolactin is lost. This renders them less efficient to produce adequate amounts of cortisol, and might lead to adrenal fatigue. Testing the cortisol to sex steroid hormones ratio easily tells us if this is a clinical problem. I do not advocate treating this without testing at all. I also use DHEA levels to do this in “more fit” or “ripped” people, because it is even more accurate in diagnosis in my experience. Evening or night-time stress is a very strong stimulator of cortisol secretion, and quickly depletes the adrenal supply of cortisol. This results in decreased cortisol levels for the next morning at a time when the serum level of cortisol should be high. This is one of the most common findings on salivary cortisol assays.
What about cortisol supplementation?
Cortisol supplementation may provide one of the most rapid improvements of all the hormone replacements. The one thing to pay attention to is that bio-identical replacement is a better choice than synthetic options. This is due to the optimal chemical transduction at the receptor level related to an oddity of proton spin. Moreover, the bio-identical preparation gives a more consistent clinical result in my experience. I see many people on low dose prednisone or hydrocortisone replacement that still struggle. Often changing the med is all that is needed to help the clinical scenario. The higher the initial dose, the quicker the short-term benefit, but it is quite short lived. More often, the requirement for reversal is low doses with over many months to ramp up to effect.
Patients on cortisol therapy may improve during the first days of intake, but complete recovery from physical signs and symptoms of cortisol deficiency takes more time in most cases in my experience. With patients who have slower response to therapy, optimal results may take as much as two to three months. If someone requires long term replacement, the physician has to seriously consider the long term pituitary effects of HPA suppression. These are very serious clinical matters not to be managed without a physician in my view.
Often a lack of clinical response is most often attributed to a poor diet. This is a diet usually high in carbs and PUFAs in unison, and low in all fats, classically described as the SAD. Therefore, the patient should be encouraged to migrate to a Epi-paleo palate as a way of accelerating the progress of healing. Epi-paleo Rx is the quickest way to destroy the cytokine storms that destroy cortisol and the gut barrier, BBB, and the lung’s barriers. It also decrease IL-6 to improve sleep and DHEA levels.
Once treatment has begun, fine-tuning the dosing means finding the optimal dose for the patient and not a dose that is slightly too low or too high. This process is primarily achieved by carefully checking physical signs and symptoms and much less by relying on lab tests. The optimal dose is the dose that relieve the patient completely from the symptoms of cortisol deficiency without causing any signs of cortisol excess. Dosing by lab testing usually helps to mitigate severe over or under dosing during treatment, but I have found them less helpful for the fine tuning needed clinically. I find paying attention to the clinical symptoms is paramount to accurately treating the patient issues. The optimal dose may vary following changes in the need for cortisol.
Cortisol can usually be started at an estimated dose based upon clinical symptoms. This is how a clinician treats the effect of the steroid at the receptor level. Most serum cortisol, all but about 4 percent, is bound to proteins, including corticosteroid binding globulin, CBG, and albumin. Only free cortisol is available to bind to receptors to give the clinical effect. The minimal efficient dose in most women is usually 15 – 20 mg per day. In men, it is greater, about 30 mg per day, usually divided in at least two separate doses. One can be given in the morning and one at noon to follow the normal circadian rhythm of cortisol.
There are two other fundamental contraindications to cortisol supplementation.
- If you do not need it, you should never take it. This must be based upon normal salivary cortisol assays, and not just symptoms! If there is no salivary testing, no Rx should be given a period for bio-identical cortisol. I take it further. I do not advocate any Rx for cortisol, even if one has an abnormal serum cortisol level over a salivary cortisol assay. Serum cortisol levels are notoriously inaccurate while salivary testing is very accurate. If one is not sure of the true level at the correct time of the day, cortisol treatment will not optimally help the patient and may cause harm. I use natural signaling to restore the cycles.
- Cortisol supplementation should not be a first line treatment option if other hormone deficiencies exist. Repairing the light exposure via the retina should be the first move. This is the predominant reason that I do not see a big clinical need for cortisol replacement often. I personally have never seen a patient with an isolated cortisol problem unless they have a pituitary, adrenal, or carcinoid tumor that secretes cortisol in some fashion. In cases like these, even appropriate replacement doses of cortisol may cause harm. It becomes imperative that a thorough history and physical for endocrine abnormalities is done in all cases. If the patient does not have sufficient levels of anabolic hormones such as DHEA, and the sex hormones to counter cortisol catabolic effects the balance of this system can be altered with consequences. The catabolic effects of cortisol can cause excessive breakdown of the tissues of the body. This is classically seen in the loss of muscle, bone, and cartilages of the body. Some of the clinical findings we see are is sarcopenia, osteoporosis, skin atrophy, ecchymosis, petechia (spider veins), and immunosuppression. I am very leery of using cortisol to treat cases of adrenal fatigue because of these findings. Adrenal fatigue is a brain stem disease and not an adrenal disease at its core.
What are the signs of cortisol insufficiency and excess?
I have covered the signs and symptoms of adrenal fatigue in a blog post, What might Casey Anthony and OJ have in Common?
The most common finding is obesity (hypercortisolism) is truncal obesity. This signifies a lot of abdominal fat and the presence of fatty liver disease. The effects of cortisol are relative to the time it is raised. This is the context that it must be placed in during a bio hack. The principal mental and emotional signs and symptoms of cortisol excess after several hours to several days are overly emotional, excessive agitation, euphoric, insensitive to human suffering, a craving of stress and often creates their own stress to satisfy their physiologic needs, stressing others out to create an environment of stress but not stressing themselves out. After several hours of elevated levels, we also see a significant reduction of thyroid and insulin levels in the adrenal gland of the same patient. Insomnia is often a critical finding in elevated cortisol cases, and is commonly tied to very low DHEA levels and low melatonin levels. Women tend to show significant defects in pregnenolone and progesterone with increasing age or sleep problems.
The principal physical signs and symptoms of cortisol excess after several consecutive days are, cardiac erethism (heart pounding in the chest) and or anxiety. When this effect persists, we can see swollen hands and feet, swollen face especially around the eye lids, elevated basal blood pressures are very common as well. After several weeks to several months of chronic cortisol elevation, we commonly see, excessive weight gain, frank morbid obesity, ecchymosis or easy bruising of the skin, petechiae (tiny skin hemorrhages) before cortisol cycles crash and flatline. After six months we see atrophic skin, altered immunity, and severe osteoporosis develop. With chronic severe elevation, we can also see chronic adrenal fatigue in some people. These last two symptoms often occur in patients where the physician does not expect to see either clinical finding as well. I personally have seen more osteoporosis in younger patients than I was ever taught to expect, so I am very cognizant of looking for this. The skin issue is seen when we close many of their surgical wounds if the surgeon is paying attention. Another sign I see is the fat replacement in the muscle bellies that are adjacent to my surgical planes of dissection. These are the clues I use at surgery to consider what the patient’s underlying physiology may reveal. Often, I gain these insights by thoroughly reviewing the patients MRI’s that they come to me for spinal disease. Rarely, does the radiologist mention these abnormal finding,s because I think they have become so common that they are not felt to be that abnormal. It is akin to a “crying wolf” scenario and requires the clinician to be very aware of what chronic excessive cortisol can do. Often the mental, emotional, and obesity effects on cortisol are ignored by healthcare providers. In my clinic, I believe that over 90{a7b724a0454d92c70890dedf5ec22a026af4df067c7b55aa6009b4d34d5da3c6} of the cases I see have a cortisol etiology at its core.
When someone is stressed and has an altered cortisol level, one could consider adding B6, Mg, and CoEnZ Q10, L-carnitine, and D-Ribose as adjuvants to therapy if they are on a suboptimal diet, but there are smarter moves to make first. I also like to see B12 levels that are high and hovering above 1000 pg/mL with a low homocysteine level and low calcium index score. I also look for greying of the hair and increased wrinkling of the skin to see how a cortisol level maybe affecting other hormones in the cascade. Chronic fatigue is another symptom to pay attention too as well for hormone cascade abnormalities which links to the spin rate of the ATPase.
Your Shopping List for this Post
 |
 |
| Life Extension Neuro-Mag Magnesium L-Threonate |
Life Extension Super Ubiquinol CoQ10 with Enhanced Mitochondrial Support |
 |
 |
| Life Extension L Carnitine |
Life Extension D-Ribose Tablets |
Additional Resources
- Brain Gut 6: Epi-Paleo Rx
- Brain Gut 11: Is Technology An Achilles Heel?
- Brain Gut 16: Adrenal Fatigue Rx
- Hormone CPC #1: DHEA
- Your VAP = Brain Gut Axis Function
- What might Casey Anthony and OJ have in Common?
- My Leptin Prescription
Cites
- F. A. J. L. Scheer and R. M. Buijs, “Light affects morning salivary cortisol in humans,” Journal of Clinical Endocrinology and Metabolism, vol. 84, no. 9, pp. 3395-3398, 1999.
- http://jbr.sagepub.com/content/25/3/208.abstract (effect of bright light on human cortisol levels)
- R. Leproult, E. F. Colecchia, M. L’Hermite-Balériaux, and E. Van Cauter, “Transition from dim to bright light in the morning induces an immediate elevation of cortisol levels,” Journal of Clinical Endocrinology and Metabolism, vol. 86, no. 1, pp. 151-157, 2001.
- Thorn L, Hucklebridge F, Evans P, Clow A. (2006). Suspected non-adherence and weekend versus week day differences in the awakening cortisol response. Psychoneuroendocrinology. 31(8):1009-18. PMID 16876958
- A b Schlotz W, Hellhammer J, Schulz P, Stone AA. (2004). Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom Med. 66(2):207-14. PMID15039505
- Steptoe A, Cropley M, Griffith J, Kirschbaum C. (2000). Job strain and anger expression predict early morning elevations in salivary cortisol. Psychosom Med. 62(2):286-92. PMID 10772410
- Rohleder N, Beulen SE, Chen E, Wolf JM, Kirschbaum C. (2007). Stress on the dance floor: the cortisol stress response to social-evaluative threat in competitive ballroom dancers. Pers Soc Psychol Bull. 33(1):69-84. PMID 17178931
- Grossi G, Perski A, Ekstedt M, Johansson T, Lindström M, Holm K. (2005). The morning salivary cortisol response in burnout. J Psychosom Res. 59(2):103-11. PMID 16186006
- De Vente W, Olff M, Van Amsterdam JG, Kamphuis JH, Emmelkamp PM. (2003). Physiological differences between burnout patients and healthy controls: blood pressure, heart rate, and cortisol responses. Occup Environ Med. 60 Suppl 1:i54-61. PMID 12782748
- Pruessner JC, Hellhammer DH, Kirschbaum C. (1999). Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 61(2):197-204. PMID 10204973
- Mommersteeg PM, Heijnen CJ, Verbraak MJ, van Doornen LJ. (2006). Clinical burnout is not reflected in the cortisol awakening response, the day-curve or the response to a low-dose dexamethasone suppression test. Psychoneuroendocrinology. 31(2):216-25. PMID 16150550


Thanks. You were right; it did shed light on how cortisol ties in with sex hormones and belly fat. So, is it low hormones that causes high cortisol, and ultimately low cortisol, or is it more of a chicken and the egg thing?
Do you have experience with ANSAR testing? If so, can you explain how a high parasympathetic response shows high cortisol, and a low sympathetic response shows low cortisol? I first had high parasympathetic, and now a year later (with weight loss, primal eating, and recently leptin reset) have low sympathetic. Doc said he is expecting low DHEA results from blood test. Is it really so simple as increasing DHEA and morning light that will ultimately help both adrenals and thyroid function?
@DrMommyN When I think about AF I always go light, hormones, and carbs in that order. Rarely will I go in another order.
Hi Dr. Kruse,
I wanted to know your thoughts on Cushing's Disease. Have you seen it in many of your patients? or is it pretty rare? I recently had my morning cortisol levels checked by my doctor after taking 1 mg of Dexamethasone the night before my am blood test. The salivary test wasn't an option, otherwise I would have done that. I was ready to go ahead and use the lab that you recommended to me to get it done, but then I went to see my doctor to go over my lab work.
My results came back as 5.1, which she said was higher than it should be given that the dexamethasone should have suppressed ACTH production and decreased my cortisol production. My doctor is sending me to an endocrinologist and they are having me do a 24 hour urine collection to test for Cushing's Disease. I am rapidly gaining weightwith no apparent reason, even while eating Paleo and doing the Leptin Reset, and have had quite a few of the other symptoms associated with Cushing's disease for several years now.
@Lauren You are describing the dexamethasone suppression test. This is a test we often do for a pituitary adenoma that is secreting ACTH. This is called Cushing's Disease and neurosurgeons are very familiar with this because we generally have to operate on most of them to reverse the disease. This is a special cause of an elevated cortisol that is much more rare than what most patients or doctors will see in their lives. Cushings Disease is life threatening and needs aggressive treatment. I would still consider getting a salivary level because it will tell your surgeon when you are secreting the most ACTH during the day. I have used this information to do their MRI and their surgery at the time of the day that the tumor is most active because it will make treatment easier. ACTH secreting adenomas are notorious in my world because often they are hard to find and can be missed at surgery and require another procedure. There is medical treatment available for this disease but it is not very responsive to it often.
both of these links are not working:
People most at risk for adrenal fatigue are those with poor gut/liver function and they usually are LR or have low HDL's on lab testing. I covered this in previous blog here.
VERY NICE!!!! I am extremely grateful for your remarkably open-sourced materials and big phat #*()@$ brain.
Yes carbs aren't always the answer but somehow Schwarzbein does work — you discussed the 'ratios' of hormones above and I concur — for adrenal fatigue when the serum INSULIN eclipses the serum CORTISOL, some magic does happen. I don't get it but it does work for some or many.
Also I totally concur — using bioHRT for adrenal fatigue (hydrocortisone) should be LAST RESERVED route of treatment until all other manners of therapy are first exhausted:
–circadian rhythm establishment (AM sunlight or spectrum light bulb)
–melatonin in the PM and avoidance of artificial lights (computer screens, iPads, fluorescene, blah blah blah)
–cofactors for the adrenals (activated B vitamins B12 folate/MTHF, P6P, etc) and support
–adaptogens
–as tolerated DHEA, preg, progesterone, etc
Thank you for stressing the importance of syncing up the SCN (suprachiasmic nucleus) to the rest of the brain-HPA-gonad-gut axis.
Brent's mentor Marc Simonson made me realize the importance of this VERY valuable and vital ORGAN. HOpe to hear more about it as well~!!!
Looking forward to the remainder of the future series!!
UR THE BEST!!!!!
Much love,
G
@Grace I am not down on carbs……i am saying clearly give the light a chance before you go straight to carbs. I have seen too many go to carbs and help their AF only to wind up with new problems that they must then solve. When one uses light as a first line treatment I have rarely seen a major problem. Its a conversation point for us all to ponder
Is artificial light good to use if we don’t have much sun here? Ty!!
I would tell you that is a BIG DEPEND on where you are and your current state. Read the Ubiquitination 24 blog and the entire Time series to see just how detailed this all is.
Fantastic Post. Couple of questions. For those of us using computers during dark periods, is it any benefit to install F.lux (which adjusts monitor display colors) during darkness? http://stereopsis.com/flux/
Second question. Regarding Dairy (Raw Cheese/Milk). You mention above a need to remove that due to a tie in for Cortisol modulation. Can one who tolerates Raw milk still consume same w/o any risk of adjusting Cortisol in a negative way? My levels @11pm on recent test were 0.049ug/dl.
Finally, during winter months, do you suggest adding a daily morning walk – even in cooler mornings to garner sunlight into the retina (when available)?
@Kevin I advocate this type of use. But honestly we should all consider turning off the electronics at dusk for the light and EMF issues. Even paleo folks have neolithic leanings that rob us of optimal. As you know I advocate AM warning light anyway you can get……walking or the hot tub!
@Chris This is a great question. High cortisol levels cause a lowered Vitamin D level because Vitamin D is the last hormone made in the hormone cascade from LDL cholesterol while cortisol is a more proximal one made in the same pathway. This is a called a pregnenolone steal syndrome. When cortisol is high is causes Vit D to fall and this directly disrupts the intestinal brush border to cause a leaky gut. The second effect is to alter the gut immunity in the GALT that lies directly below the brush border. This alters the conversion and maturation of T cells I spoke about in my Vitamin D post and in the leaky gut series. Once you have a leaky gut neurotransmitter problems quickly follow as I laid out in my blog on neurotransmitters. This sets up the brain for many diseases and not just depression. This is the essence of the brain gut axis and why I have this as a levee all its own in my QUILT
Great post. Just wanted to say thank you for these recommendations, I've had some great results from making sure I get more sunlight in the mornings and throughout the day. I'm tapering off prednisone and have been struggling with major fatigue but restoring my circadian rhythm has really helped with my mood and energy levels.
@Shah Your email about steroid weaning is a great one. As a neurosurgeon we are very used to weaning steroids often. I also use other hormones as a taper adjunct and i have now begun to use light and light boxes for those who can afford them. When I was a resident I was not trained on how to really taper steroids. I was taught how most do it using a decreased dose over 7-10 days. That works but it usually leaves the person on them with altered hormonal status. This is especially true in a case like yours when we use the Bracken protocol for a cord injury. I am glad to here that your injury has reversed and that my advice on heavy cold use and progesterone cream helped you. Keep me informed of your progress and new MRI results. I have a surgeon here locally who went through a very similar story to yours that I will be soon documenting.
I fully concur with
grace (Dr.BG)
————————
She said:
1–Also I totally concur — using bioHRT for adrenal fatigue (hydrocortisone) should be LAST RESERVED route of treatment until all other manners of therapy are first exhausted:
2–circadian rhythm establishment (AM sunlight or spectrum light bulb)
3–melatonin in the PM and avoidance of artificial lights (computer screens, iPads, fluorescene, blah blah blah)
4–cofactors for the adrenals (activated B vitamins B12 folate/MTHF, P6P, etc) and support
5–adaptogens
6-as tolerated DHEA, preg, progesterone, etc
————————
But
from what I see being discussed on bb's, #1 is used mostly (often synthetics)
#6 is used least, worst, progesterone is used first and that clouds the whole picture,
#5 is ill defined and hard to check if they brought in any added value
I have seen statements that the term AF (Adrenal Fatigue) is inacurate, actually misleading.
Most of the time adrenals are not fatigued at all, they just either do not have the raw material or nobody is asking them to produce.
Comments?
I know that glass blocks certain of the sun's rays – UVB, I believe? or is it the other way around? What about contacts? Can I get the effects of the sun on my retina if I always have contacts in?
@DrK, I think this may be my problem. I've been trying to solve my hypothyroidism for months now without any luck. I'm 31 and have taken birth control for about a decade which I stopped around 8 months ago due to unusual spotting, plus I want to try to have a child soon but I haven't menstruated since! I've had problems with depression and fatigue for many years but no medication ever helps. I wake up with puffy eyes and can barely drag myself out of bed to work. I've been constipated for years but it goes back and forth and I probably drink too much alcohol every night because it's the only way I can deal with how crappy I feel everyday. I found both your website and the PHD around 6 months ago and started eating more organ meats like liver and trying to eat more saturated fat i.e. coconut oil as well as supplementing VitB's, Se, Mg, VitC, VitD, melatonin, plus working up to a high dose of Iodine, 25mg right now. Before that I had already been eating VLC paleo, no salt, no processed foods, lots of veges and quality eggs and meat for the past year or more but my health has only declined: high TSH, low T3, low T4, high rT3, low estrogen, low progesterone, high prolactin, normal DHEA, very low VitD levels, and earlier this year 1 blood test showed some elevated liver enzymes yet I've had multiple MRI's, endoscopy, colonoscopy, etc and no one can find anything wrong with me. I try to force myself to exercise but I dread it so much that I rarely do, although I wasn't exercising much to begin with and I've only been gaining weight, I may be 30lbs overweight now, mostly around my waist, and I still seem to be gaining =(
Finding a good Dr in the Orlando area has been tough but I have a "decent" one who has prescribed me Synthroid, although it did nothing after 2 months, so he switched me to Armour and it made me feel hyper the first few days but since then it's done nothing for me in 3 weeks. A few months back at the recommendation of Paul from the PHD I started adding some starch into my diet from white rice and my constipation immediately got better and I honestly thought I was slowly starting to feel a little better some mornings. But my weight kept going up so I dropped the carbs a couple months ago and went back to VLC and I've only gotten worse. Constipation returned, still gaining weight, dry skin and hair, always cold, lightheadedness, low basal body temp that changes everyday, can't get enough sleep and wake up constantly, and I always feel very stressed and very depressed. I just called my Dr to ask for a salivary cortisol test but his office didn't seem to know what I was talking about and they haven't contacted me back.
Your article I just read this morning worries me because just yesterday I read some stuff from DrBG and came to the conclusion that the increased carb intake I tried a few months back may have actually been the "magic bullet" and so I decided to again start getting 50g-100g carbs per day from white rice. It's the only thing I've changed that was associated with improved symptoms and after I dropped them my symptoms got worse again. I've tried VLC for so long and it doesnt seem to be working. I hope you're wrong about carb intake because I can't take feeling this way anymore and I'm only getting worse!
Hi Tiff, what was the solution to your problem? Did you figure out what was causing the weight gain? If you can, please update us, thanks!
Dr K yet again another amazing post. Reading it I could easily link back my cortisol issues & pregnelone steal syndrome back to college & the stress of carrying 21hr course loads + competing on the swim team for 4 yrs. add that to working graves & swings while in the military and the ground work for AF was set. Add in working emergency response looking for the high tempo & associated stress. Coupled w/an inability to loose weight i gained over that time period, boy did I set myself up for this. It's taken close to 7 yrs to get where I am today but have a long was to go til Optimal. Looking fwd to my next salivary cortisol test in Jan to see where I'm at. I positive I'll see normal results as I'm waking up refreshed & w/in 30 mins I'm operating @ 100% w/o even considering coffee. My am decaf is sometimes an afterthought
Thanks so much for all the work you are doing. You're changing pols lives real time!!!
Thanks! I lost my sunglasses about a month ago, and still haven't replaced them. But, I am finding that due to a tonic pupil, being without them without a wide-brimmed hat gives me some difficulty for the one eye. I am also finding the wrap-arounds protect my prescription glasses from damage and also keep my eyes protected from dehydration and wind damage. Is there a specific wrap-around color that would be better than the typical grey?
First off,your generous contributions, information and patient support are greatly appreciated.
I've been on the Leptin RX for about 8 weeks now.
The question is for light timing and cortisol reprogramming. To rise with the sun here in South Florida is around 7:30 am., so this is when I eat my BAB. My question is for the evening time. It gets dark rather early now (5:45)ish, and I'm able to finish dinner between 6-7 pm. What do you recommend for evening activities between 6-10 such as eating or reading without using artificial lighting?
@Jenni using a blue light or red light to read. I recently mentioned in my JoanneUnleashed.com podcast that I read with a red/blue hunting site attached to a baseball cap often. I am doing it right now. I also have screen filters on anything with light and I no longer watch TV after sunset much. I don't even use an LED clock in my bedroom. Night time is for teaching your young one's how you might become optimal if they change. Sit them in your lap and talk to them. Im teaching my kids now to become mindful at night. If you don't have kids…….cuddle up to your lover. Then well…….make love. If you dont have a lover you can find one in many adult toy stores that dont have lights to meet these needs. We all need as much oxytocin as we can get. And if you still are bored…….buy a hot tub and look up at the night sky and enjoy the natural light of the sky and see the wonder out there that can motivate you to become one with your own built in optimal self. Listen to Pandora and make a mindful playlist…….Listen to your brain think as you allow it to do the things it was built to do in the dark…….before we built our new neolithic environments to detract our attention from the real prize. Night time is when we do my best work thinking if we allow ourselves the time to. I am very sharp at night because I am living with our biologic rhythms in light and timing. My internal light shines best when I am thinking in pitch blackness of night.
Dr. Kruse,
I have been doing the reset for a few weeks now….thank you so much for your blog and all you do.
I have a few questions about already being on hc and trying to wean off. I have been on hydrocortisone for years for AF (doctor gave me diagnosis of addisons recently because blood work done showed extremely low cortisol even on hc). I was on 30mg, but have now brought my dose down to 25mg taking away my night dose. What is happening is that I go to bed and to sleep by 9:00-10:00, but I wake up when it's still dark outside at 5:00 am. I have developed severe back pain that happens only in the mornings and I cannot stay in bed no matter what I do. I bring up the back ache because I'm almost sure it fits into this somehow.
Am I doing the right thing or do I wait until I know I am completely sensitive to wean off of anymore hc?
@Michele Anyone on HC that long is going to wind up adrenally suppressed. Moroever, that is the source of your back pain. Just google JFK AND back pain. I hate hearing this kind of story. All neurosurgeons and spine surgeons know about the spinal damage caused by Addison's. You will also notice browning of your mucous membranes and in your mouth, vagina, labia and nipples too. Your skin may also be browner than it was when you were younger. These signs should have been picked up long ago that a new approach was needed to treat your AF.
I have severe adrenal fatigue with low cortisol all day. I am currently taking 30 mg. of hydrocortisone per day in divided doses. I am also on T3 for a high reverse t3 and a conversion problem of t3 to t4. I bought a full spectrum lamp a few years ago for seasonal affective disorder, but have not used it in awhile. I wake up at 5, about an hour before daylight. Should I sit next to my full spectrum light when I wake up? If so, for how long? I also have one of those lamps that gradually comes on to help you wake up to simulated sunlight? Would this be beneficial to use? Thanks so much!
@Sandy You should always follow the light cycles evolution/GOD provided us with. If you want to use the gradual light box I think this is a better choice. Me…….I will remain waiting daily for the AM sunrise from my hot tub as I think and listen to what my brain is telling me.
Great blog, Dr. Kruse.
Among other problems…I have high TSH, high RT3, very low Free and Total T3. Previous attempts to supplement with T3 were unsuccessful (made me feel worse). My doctor placed me on Hydrocortisone with the goal of lowering inflammation to allow me to better tolerate T3 supplementation.
I started out with 15mg HC in the morning and 15mg at lunch time along with 10mcg T3 (this was the most amount of T3 I was able to tolerate). My Free T3 and TSH improved slightly but my RT3 raised from 385 to 464 (90-350). What do you make of this? Shouldn't RT3 have lowered given the HC/T3 supplementation? Does this indicate that I need more HC? I've since added a 3rd dose of HC 10mg around 5pm.
Another thing I found interesting was that my progesterone levels actually improved from <0.1 to 0.4. I would think adrenal suppression from HC would lead to lowered Progesterone levels but perhaps Progesterone is now being spared?
@Dru Sounds like you have a mix of hormone issues from both the autonomic nervous system and the brain not in balance. You need a doc who understands allostatic balance and symphony of optimization. Look into an age management paleo doc in your area. That will help you immensely. Good Luck and keep me in the loop.
I often hear Sisson and others describe "chronic cardio" and they all say it leads to high cortisol and belly fat that won't budge. Is this just bro-science or is there something to it? I have seen many clients that stall on weight loss only to start losing again when they lay off the daily 2 hour walks or 30 minute jogs. Is there a connection between cardio-induced cortisol and stubborn belly-fat?
@Primal Trainer Not only is there a connection but that connection is direct. If you perform chronic cardio you diminish your stem cell depots and you age faster and your telomeres shorten faster. A nobel Prize got handed out in 2009 for these insights. If Mark Sisson, Art DeVany and Robb Wolf all report the same thing…….you can book it. I have future blogs on this very issue in the que. The 2010 article showing 100% of long term marathoners have myocardial fibrosis in is pretty epic. Moreover, Sisson is a former world class runner. Id say he knows the science and has the chops in this area. It's also why EMS is required at every marathon by law and not at any weight lifting competition. Kinda makes you wonder why? If lawyers know why don't you?
Dr. K. Excited when I saw this post, but still can't seem to figure out what course of action I need to take. I have had weight problems and bouts of fatigue since I was in my 20's. Now I'm in my early 60's. Over the years, both got worse. Doctors never could find anything wrong.
I finally I have a doc who I am making some progress with, but so far it has just been finding rather than fixing. Vit D is now OK, but that's about it.
Low testosterone, low DHEA, low cortisol (saliva test), high blood pressure, high rt3, and insomnia. Tried testosterone cream and it only slightly raised t level. Stopped when I had a cancer scare from an elevated psa.
Tried cortef (25 mg) for about 6 weeks and ended up with severe headache that wouldn't go away. Stopped the cortef.
So now I am taking a couple of adaptogens, b6, zinc, magnesium, selenium, and a bunch of other supplements. I am doing the leptin Reset. I have also added in supplements you recommend for leaky gut.
So am I on the right track? I'm assuming the first things to do are the Leptin Reset and fix Leaky Gut. What else should I do for high rt3 and low cortisol? I have had the cortisol lab twice and all 4 times were low both times.
@Rich The right track is to get hormonally right and eat to stay that way. That is as simple as I can can state it. Do many need a Physician health coach to do so……..Sadly based upon my blog comments the answer is yes. But my life's goal is alter that. And trust me I am working on this big time with some people you know well.
What about increased cortisol from VLC, and the need for the liver to undergo gluconeogenesis? So assuming one is healthy or becoming LS, would you agree or disagree with Paul Jaminet's 20% carb intake?
@Dan Han There is no abnormal cortisol response from VLC eating Dan. This is the normal and expected response. I mentioned that in this blog. The liver needs to use gluconeogenic pathways for us to get to optimal. Where do safe starches play a role……? Those who are completely healthy who can handle all dietary macronutrients (pretty rare people) because they are metabolically efficient while being hormonal balanced. Those who "feel" they need 20% carbs to "feel better" because they are not close to optimal because of severe underlying hormone imbalance. My job is to figure out which camp you're in as a patient. If you blindly follow a "perfect starch methodology" without testing…….you're driving on a road with a balcked painted windshield hoping the road is straight and clear ahead. Our evolutionary machinery has an exquisite hormonal synergy. Each instrument has its own melody or rhythm, but all are necessary to play our life's orchestra. What way you play your music is for you, the composer to discover. Me………I think I'd rather be hormonally optimal and limit my carbs to my light cycles and nature built in.
Last year I used HCG to lose 20 lbs which had slowly crept on during my 40's. From that hcg forum I stumbled upon your site (which I find fascinating) and started transitioning to your leptin rx. When I finished the HCG I continued with low carb as it made me feel much better (more energy, less foggy thinking). I may have already been LS at that point, I'm not sure, but I started your reset anyway, hoping to seal the deal. It has really helped with cravings, being able to go long periods without food if needed, and an increased sex drive. All good. However, the one problem I have had the last several years has been with sleep. And this continues to be a problem. I have seen a sleep doc who put me on Celexa, only to make things worse. Melatonin dosen't help. Benadryl is like a sugar pill. I have Lunesta and Ambien which I hate to use but often have to. I found a functional med doc I like. She thought it had to do with low progesterone and had me go ahead and start low dose progesterone before salivary testing (my choice). Seemed to work for a few days and then suddenly I became much worse, and had increasing anxiety during the day (50 mg then 25 mg dose po). So I stopped. Incidentally I have tried a very low dose of pregnenolone 6mg for a few days do see if would improve cognitive function only to have the same anxiety provoking response. Any thoughts on why everything seems to shunt towards cortisol? I have an appt to have my salivary hormones tested in several months. But wondering what to do if it shows I need progesterone even though I seem unable to take it. My doctor states she has several pts that even though tests show they are low in progesterone, they are unable to tolerate even low doses as it seems to induce anxiety. She is not sure why this is. Im 47, still with pretty regular menses, no hot flashes. I lift weights and do short cardio 3-4 times a week and have for years. I supplement with vit D, magnesium and B complex. Any thoughts? Suggestions? Thanks so much for sharing all of your years of hard work and your brain power with us! So much time and effort you put into helping others…it is so appreciated
@Vicki bad sleep is usually due to low DHEA or progesterone production. Get those tested and optimal to the top quartile of their ranges and I bet your sleep improves.
Just wanted to say thank you for your informative, superbly well-written blog.
And to let you know that I think you should write a book and CHARGE people for it!!
I've read Dr. Eades for years (got me on the LC bandwagon), but reading your blog cements everything in place.
A couple of years ago, I WAS having terrible ammenhorrea; multiple large fibroids; OB/GYN offered to practically drive me straight to the hospital to take it all out. I declined, did a ton of research, where I found LC, Omega 3's, etc. LC'ing and adding Krill oil daily (per Dr. Eades' blog), the ammenhorrhea is gone. Just…snap….gone. And I got to keep all my parts. 🙂
But, I still couldn't keep the weight down (5'2" female, almost 50 yrs. old, hover in the high 150's/low 160's). I'd LC, do great, then carb-binge. Rinse, repeat.
I KNEW I had a leptin issue, but couldn't find enough info on it, until I found a link from another LC site that led me to your blog.
After devouring your blog:
I've been making Leptin Reset adjustments: BAB, NO snacks, mostly protein and Omega 3's, only carbs are cruciferous veggies, trying to work more with my circadian rhythms and establish a better sleep-wake cycle.
I WAS waking up at 2-3 a.m., turning the t.v. on, back to sleep around 4 a.m. Also was having night sweats. Of course, my OB/GYN and my friends assured me it was all perimenopause, even though I still have regular periods with no more ammenhorea.
While on Leptin reset, it's been almost magical: the sleep? I woke up last night, middle of the night, but didn't check the clock. Turned back over, fell back asleep. No "middle-of-the-night" t.v. needed. Haven't had the excessive sweating either. I'm thinking this will get better as I continue on the LR.
To be honest, I don't know if I'll ever become truly LS, as I've been a true carb binger my whole life. Not being a slave to a package of Oreos has become a godsend.
154.4 lbs. this morning. Down from 162.8 two weeks ago. I know, I know, I shouldn't scale-watch, as it increases cortisol. Still working on that one. 🙂
Dr. K. even being on hc this long, is there any chance I can slowly wean myself off it while doing the reset?
I can't live like this much longer. The back pain is excruciating. Is it too late for me to reverse this? I am so scared now.
I am really considering a trip to see you soon.
Since it's going to be a few months before I'm able to test my hormones, I think I am going to go ahead and try 25mg 7 keto dhea for sleep (per your answer above) as I know that the progesterone just causes anxiety and worsening insomnia for me, for some reason. My question is…as 7 keto dhea, as I understand it, is a metabolite of actual dhea. Would I expect supplementing with 7 keto to be reflected in my future dhea test or not? In other words will I expect it to raise my dhea-s? And if it does help me with sleep, is the effect immediate or will it take awhile? Again, thankyou thankyou for your thoughts
Vicki, did she put you on BIOMIMETIC progesterone or PROGESTIN (synthetic)? They are NOT the same thing.
I started using natural progesterone cream a decade ago and the very first day I used it I slept for 8 hours. I had been sleeping two hours a night for over a year. No exaggeration. I continued the OTC cream until this summer when I found a Wiley Protocol provider and went on full biomimetic hormone replacement therapy. It has been THE best thing I have EVER done for myself.
Now, even though I'm battling through the leptin Rx (decades of an eating disorder to deal with) I am now sleeping like a baby. My head hits the pillow and I'm GONE for 8 to 10 hours. It's WONderful!
Dr Kruse,
As you say, it's rare to find an isolated Cortisol deficiency in Adrenal Fatigue,
Do you believe that Adrenal Fatigue is just, more or less, a Burn Out situation where there is a multi hormonal deficiency triggered by stressors in daily life and work(unhappy relationship, marital or not) and abnormal circadian rythms (lack of sunshine, night shift, computer work…).
@Esochiro60 I think adrenal issues are always complex and most people try to make them simple with recommending carbs to fix it. You must draw labs and know precisely how to diagnose it and treat it by slowly reversing all the issues found.
@darleen. No it was progesterone, not progestin. My doc says she has a few women that react the same way I did and she isn't sure why. Wish I knew. I used to be one of those who slept like a baby until the last couple of years. I always took it for granted, never thinking sleep could ever be a problem for me! Gonna give the dhea a try. Fingers crossed and thanks for your input.
Sorry to be a bother, Doc, just wondering if you had any insight on my question above. I never know if my walks with contacts in are pointless, and maybe I should have glasses on (which allow unfiltered rays in from the top) for that short time each morning instead. Here it is again:
I know that glass blocks certain of the sun's rays – UVB, I believe? or is it the other way around? What about contacts? Can I get the effects of the sun on my retina if I always have contacts in? Do you need the full spectrum (which is not available through windows) to get the benefits?
@Mamagrok This is a question to ask the optometrist who filled the Rx for the contacts to tell what it blocks. I have no idea about contacts because there are so many lenses.
Vicki, might I suggest you get a copy of "Sex,Lies & Menopause" by TS Wiley et al. It's a REAL eye opener!
Interesting; I didn't know it would vary. I imagine that the full spectrum isn't required since working near a window suffices, I think you said? Thank you!
Dr. Kruse,
As per above, addisons brought on by corticosteroid use with severe back pain, do you think vitamin k, vitamin d, the reset and trying to wean off of hc are my best bets? I know you don't like to answer straight up questions like this because I'm not your patient ( I will be soon if I can help it), but I have no one to turn to. You seem to be the only one who gets it. I thank you from the bottom of my heart even if you don't answer. Just doing the reset so far has changed so much for me.
@Michele With Addison's disease there is little chance of coming off steroids. Addison's disease is a life threatening disease that must be taken seriously with a doctor's help. I would strongly recommend you lean on your on MD's for treating this disease. I think you trying to do everything you can do to be healthy is a great idea. Eating Paleo and monitoring your health is critical to getting your best results.
It's the back pain I can't handle.
Thank you Dr. Kruse
@Michele. If that is the case have your doc refer you to an anesthesia pain specialist to help you out! Optimizing your diet and K2 D3 and will help for sure
I just read a very intriguing study done recently on the affect of mindfulness and visceral obesity and stress done at UCSF. Jack, what you have been saying all along about the mind connection in all of this is essentially proven by this study. I encourage all to read it, especially women who can identify with stress->overeating behavior.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC31844…
Hi Dr. Kruse,
Thanks so much for all your effort and insights, I have learned much. I'm doing a lot to get my health sorted: Leptin Rx, some supplements (K2, magensium, etc), being more aware/in control of my mood/reactions, turn off the computer by 7 pm or so–and once the sun is gone I light candles/tea lights to see. I'm also getting to bed early, 10:30 at the latest. I'm still waking up several times a night and not sleeping long enough (i.e. 7 hours). Any further suggestions in this area would be appreciated but this is the main problem I'm hoping to find a solution for ASAP. I have a dog and I live in an apartment building. He needs to go for a walk at night before bed. It's not usually long–max 1/2 hour (usually less) and it really is a saunter more than a walk. I enjoy it because it is generally relaxing but the light is too much. Mostly its the bright lights in the hallway. I've been wearing sunglasses, but do you have any suggestions?If sunglasses are a good idea, are there better ones to wear?
@Bonita I do not think sunglasses can totally block artificial light from turning off the conversion of serotonin to melatonin. The body is very sensitive to light and this chemical reaction is can be turned off with very small amounts of light just hitting the skin. It does not require the light to hit only your retina but the retina light reflex is a a major switch for this reaction.
Edit to post # 35: Instead of amenhorhea, I meant dysmenhorea. (This is why I leave the science to people like you, Dr. Kruse!).
Question: I've been hypothyroid, on Synthroid for a few years. If my TSH tests normal, can I still become LS if I continue to follow the Leptin Reset Protocol? Or is it more difficult due to the inherent Hashimoto's?
Doc, I'm having a vague memory that carbs help produce serotonin? Is that correct? If so, would that be why carbs help some people sleep when it seems counterintuitive. But it would be the short-term unhealthy "fix," rather than real repair, similar to the hypoglycemic who takes in sugar to raise blood sugar…helpful in the immediate, more damaging in the long run.
@Mimi Sleep difficulties have many causes. For example, we need carbs with protein that contain the amino acid building blocks for serotonin to be absorbed. If you dont have enough building blocks you cant convert the serotonin to melatonin. In other cases there is a poor conversion of the serotonin to melatonin because of artificial light or because of inflammation that leads to IL-6 production. Excessive carbohydrate and PUFA diets cause this cytokine to raise to dangerous levels as well and cause sleep difficulties. The same macronutrient can be problematic depending upon the context of the situation. The same macronutrient can also be harmless to us in the right situation. Generally when we have high levels of back round cellular inflammation we have to worry about macronutrients that may cause certain biochemical pathways to become active that might hurt us in some fashion. Examples of this are IGF-1 and mTor activation being associated with decreased longevity in humans with back round inflammation.
"In my experience, people with highest risk of adrenal fatigue are generally those with poor hepatic gluconeogenesis, and not from a lack of a dietary carbohydrates. One would be wise to adjust or tighten their light cycles first, then fix their liver problems next, before they consider eating a lot of carbs to fix their adrenal fatigue first."
Working on wearing eye mask at night, getting outside at sunrise, using lightbox during day, but having hard time with no computer at night (but did install the Flux dimmer.) Is the leptin reset how you fix the liver? Or is there more?
@Dr. MommyN read the last comment I just made in Leptin Part deux blog comments……..the master controller of the liver……..LEPTIN. The research daily pours out that every human better learn to master her if they want optimal. Get Leptin right and your life will be right. That needs to be on a business card.
@angie regarding your cushing's disease. Cortisol levels vary with the diurnal cycle and also display considerable internal variability. A 24-hour urinary free cortisol is best as it reflects hormone production over the entire day, and effectively provides a global production level. A random urinary free cortisol will be subject to variability as would a blood level. Measurement of CRH reflects hypothalamic activity, not activity of the pituitary or adrenals, themselves. ACTH levels are inaccurate due variable release and to the short half-life of this hormone in blood.
event: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd…
@Jane Regarding your NP action with your salivary cortisol level testing email: Stress response to your thyroid is huge and very misunderstood by many. Chronic physiologic, mental, or emotional stress results in decreased deiodinase 1 (D1) activity and an increase in D3 activity. This causes decreasing thyroid activity by converting T4 directly into reverse T3 instead of T3. Conversely, deiodinase 2 (D2) is stimulated, which results in increased T4 to T3 conversion in the pituitary only and results in reduced production of TSH!!! So when I see somebody with a lower TSH and other crazy hormone panels I know cortisol is raised somewhere and is causing the mixed signal from the activation of the D2. The increased cortisol levels seen with any stress also contribute to physiologic disconnect between the TSH and peripheral tissue T3 levels. This reduces intracellular T3 which is a cofactor in making all the peripheral hormones from LDL cholesterol. So when some one is stresses with a higher cortisol we a higher LDL and lower HDL and low hormone conversion. The easiest one to measure is Vitamin D and DHEA. I also use ferritin, HS CRP as proxies for cortisol too. This stress induced reduced tissue T3 level and increased reverse T3 results in tissue hypothyroidism and potential weight gain, low energy with fatigue (Fibromyalgia), and depression. This vicious cycle of weight gain, fatigue, and depression that is associated with stress can be prevented with supplementation with timed-released T3. We have a lady over at MDA who struggled for 15 yrs before her docs got her right. If you know the biochemistry and apply it well you can help people.
Quote: "Testing the cortisol to sex steroid hormones ratio easily tells us if this is a clinical problem."
Could you elaborate a bit about the ratios or where to get info? I'm going to make a leap here and say that low T and low cortisol means to take supplemental T will bring up cortisol? And if that fails one could possibly have a more serious adrenal gland problem?
The LR issue and your explaination of such and the body/mind connection make a lot of sense to me in relation to cortisol issues and I am very interested in its application for my own health. I have a couple of questions I couldnt find the answer to on this site.
I have adrenal issues, am obese, have high reverse t3 and low dhea and accompanying hypoglocemia plus hormone imbalances and I averaged .5kg per week weight loss on vegan diet without feeling hungry but obviously required regularly eating a lot of vegetables (but low fruit) all day and I used beans as my protein and some nuts.
My questions are:
* Can losing weight to reach normal bmi alone recover our leptin sensitivity(whether you achieve it via paleo or other means such as vegetarian or vegan?). In similar way that insulin resistance is improved by losing weight?
* I have trouble digesting proteins due to above health issues and feel much better digesiton wise on vegetarian, should i approach the paleo diet any differently?
* Also, kidney and liver function can be affected by adrenal fatigue/high reverse t3 and related symptoms of slowed metabolism etc, how will my body go on such high protein when it struggles now on normal amounts of protein?
* Is high animal diet linked to inflammation? Vegan definitely lowered my inflammation symptoms (such as red skin etc)
Thank you in advance.
@Lani I do not think you can be a vegan/veggetarian and get any modicum of success. That manner of eating is not leading us to optimal because it is contrary to our biologic directives. In my view you will have focus in on your primal sense to direct you to repair that thinking first. Once you do migrate to a diet that will bring you to the place you seek.
1. Losing weight alone is not a cure for LS. Many people who have great BMI's are LR. LR is a function of inflammation at the brain's hypothalmus and a broken leptin receptor.
2. You have problems with protein because you have a leaky gut from poor dietary choices being a vegetarian. You need to really read my Leptin rx postscript post and see what I said about the circadian cycle for gastric acid production and how this is tied to protein assimilation and how it increase protein synthesis 400%! That blog is probably the most important one I have ever written because of the shear chronobiology is optimizes if one does it.
3. kidney and liver function will normal once you get leptin to allostatical back into control. leptin is the first hormone that must be fixed before any other. It seems no one realizes this very simple and basic fact.
4. No it is not. The vegan and vegetarian diet is. what proof? Go draw your HS CRP and Vitamin D level…….It will show an elevated HS CRP and a low Vitamin D. And then maybe you can move on to animal based paleo template as evolution prescribed for our species.
You may remember me from PaleoHacks. I quit taking Synthroid last summer. I had been taking it for 6 years. My TSH was 35 in 2005. I had high BP, high trigs, gout, fatty liver. After 8 mo on Primal Blueprint diet, I got off all meds and had lost over 50lbs. My TSH was consistantly .55 for several months while on Synthroid. A month after taking Synthroid, my TSH was 2.55. Now, 6 mo later, it is 3.6.
I'm very low carb with almost zero sunlight where I live. My D is 80 w/10,000IU per day supp. Do you think my TSH will trend back down when the sunlight returns and I start increasing carbs?
Thanks for all you do, can't wait for the book!
@Akman……..3.6 is trending up so your are getting hypothyroid but before you jump for some drugs……remember that you are in severe north latitudes and people furthest from the equator are MORE sensitive to light cycle and via a pineal thyroid tract in the brain!!!! So up your D levels and use lights and then consider drugs. Timing and light is huge.
OOOps, meant to say, 'a month after quitting Synthroid, my TSH was 2.55, 6 mo later, it's 3.6.'
Would you consider 7-Keto-DHEA as a winter supplement in the far north?
@Akman…….i think when you have extremes of the light cycle you need to do extreme thinks. Just look at the Inuit native diet as a perfect template for you. If I were in your shoes I would be a ketogenic paleo and use every means necessary to build the optimal you based upon your testing
Jack – Thanks so much for your thorough explanations. I have been frustrated at a lack of information related to my own personal health problem: a cortisol deficiency that is due to a lack of ACTH production. There is so much written about adrenal fatigue and even Addison's, but I realize this is more rare. I am a 37 yo woman who had a large pituitary tumor removed last spring. It was a prolactimoma that did not secrete prolactin, hence a protracted diagnosis. The only indication was long-standing amenorrhea with undetectable estrogen, FSH and LH. These have remained low postop, but I also developed a cortisol deficiency. I have been taking hydrocortisone 20 mg daily for the past several months, and when I get serum cortisol draws in the AM (holding the AM dose), they have not risen above 4.0. Some have said that I may never regain this pituitary function, while others remain optimistic.
The cause for the persistent deficiency is unclear, but I have since been looking for guidance on how best to both manage my current condition and optimize my chances for recovery. I would like to NOT be on steroids for the rest of my life, but if I have to, I want to minimize any negative effects they might have over the long run. Do you have any recommendations for cortisol optimization when the problem is the pituitary? I am otherwise a healthy and active. My endocrinologist had no clue when I asked about how to optimize my cortisol through diet, exercise, and lifestyle. I doubt anyone had ever asked him that before!
@Dr.D you need an alpha MSH test performed to see if its low…….it maybe the cause of the problem. Check my blog out on 1/8/2012 in the comment section there is a whole comment about the MSH test. If your low you can buy/get a Rx for a replacement hormone for it from your doc. I'd also think about your gut. You need to consider a metametrix GI fx test with your doc. Once you have your pituitary fossa opened it can become a chronic pathway to allowing inflammation to pass directly to the hypothathalmus…….
@DrK What is your opinion of ZRT blood spot for DHEA that can be collected at home. Also, I use a bioidentical DHEA cream and had a sample sent to you to try from Twist25. Seems like bypassing the liver is a good idea?
@erin I like zrt's home test…..the cream did nothing to the dhea level in my testing.
@Dr.K. Ok, so I've been reading through quite a few posts on cortisol, adrenal glands, leptin reset etc. and I think I get the basics (sort of anyway). But here's the thing I get confused as to how it would relate to me and my situation. I was born with congenital adrenal hyperplasia, the salt wasting kind, so my adrenal glands aren't weak as such they're broken from the start :P. I don't think I want my cortisone much lower, but I know my renin is sligthly low my salt levels are still good though. And of course I have a thyroid problem. Could you maybe do a blog post on how a CAH person might deal with all this? leptin, telomeres, weight, energy, as much as you possible. I just get this feeling that it's basically the same but not really. And do you have an opinion about plenadren? (new cortison medicine) Thank you!
@Lydia I will consider it. Based upon what I know to date to so far my prediction is that a congenital condition that lowered cortisol levels permanently would limit longevity and lifespan via our telomere lengths. The reason is simple. Cortisol stimulate neurogenesis in our brain's hippocampus we control's all learning in the human brain. We learn by moving through our environment and experiencing all life this way. It then builds our reality through these primitive motor/learning systems. There is no way evolution would not tie this to telomere biology at some point. Its too crucial and too primary an issue for evolution to make that error for my primal intuition
@ Dr. K Thank you! Realised now that I forgot to write that I'm on medication, have been since I was 2 weeks old. So telomeres or no, without meds I'd probably be dead ;-). Thank you again!
Dr. K – have been lurking here reading and learning a lot and am seriously considering LRx, though my nutritionist opposes (she's really pushing for the 5-6 mini-meal/day routine, though is supportive of grain free, dairy free, legume free). I have a cortisol issues, which has me a bit confused – wrapped around the chicken-and-egg axel, and I want to make a wise choice re: Leptin Rx. Here's the situation…
Recent lab work shows that I have "elevated" cortisol, but that it still follows the diurnal rhythm. And when I say elevated, I mean it. 6am- >110; noon- >110; 6pm = 62. My midnight sample had a problem so we are re-doing that now (actually running all of them again). DHEA = 6. My fasting insulin was 3, fasting glucose was 93. I also showed a problem with estrogen methylation (different set of tests), which appears to be cortisol or cortisol-cascade related. All the thyroid tests came back "normal", except that I found thyroid # optional ratios in another of your posts, did the math, and my ratios suck, but of course that's not something CW looks at, so what can I say.
I have mildly elevated blood pressure (130/high 80s), am morbidly obese (5'8" female 240 lbs), and have only 1 kidney, and to the best of my knowledge 1 adrenal gland (per CT December 2010 – didn't realize the nephrectomy in 1981 was a radical, but that's how it appears to shake out – maybe not such a surprise given that the reason for the surgery was traumatic injury that cut off blood supply). I am going for a sleep study in a couple weeks because sleep apnea could be a contributing factor here also.
I have been 100% Primal for about 6 months with zero weight loss.
MD has me taking heavy B vits supplements, D3 supplement, CoQ10, and magnesium, along with my fish oil, multi, probiotics, and hypertension med (Lisinopril 10 mg).
I know that losing weight will help lower my cortisol, but it seems as though cortisol may be what's preventing me from losing weight?!!!?!?!?
Might the Leptin Rx help me lower my cortisol? I think if I can resolve the cortisol issue, I can then have a strong foundation from which to work on the blood pressure, the estrogen methylation issues, etc.
Not seeking any diagnostics here, but any insights, thoughts, or "things to think about" would be greatly appreciated.
Thanks! And keep up the great work!
@Diane………fire your nutrionist and hire @grassfedgirlsf on twitter or Diane SanFillipo……they will turn you into a rockstar. You need the Leptin Rx too for sure. Get on the Monster MDA thread too……you will learn a lot from my peoples there.
Dr.Kruse, would you consider taking Phosphatidyl Serine for lowering a high night cortisol?
@Mart I have no problem with it. I like PS and PC for people with neurodegenerative disorders like MS.
Thank you!
where do you get the screen filters…..I am having a really hard time turning off technology after sunset.
I have off the charts low cortisol in the morning and off the charts high cortisol for the rest of the day and well into the night. I read caffeine increases cortisol. Is there an amout of caffiene that would be okay to use in the morning to strategically signal more cortisol…and to not feel like a zombie?
@brenda caffeine helps but it means there are other things wrong. Do the Leptin Rx rest and the CT. It will all get better. When you see tonights blog post……well, I think this little issue will be forgotten completely
YAY
Dr Kruse,
Day 10 of Leptin reset. Up until today I've felt like a million bucks. Then something caused me to crash and I can't figure it out!
I've been trying to reset my sleep patterns so I've gradually been going to sleep earlier and waking up earlier. Last night, after an 8pm dinner of roasted cauliflower and eggs and plenty of coconut oil, I could not keep my eyes open past 10:30. This morning I awoke naturally at 7:45 (REALLY early for me.) but I was tired. I forced myself to eat breakfast at 8:15 – a not so BAB of eggs with leftover cauliflower. An hour later my eyes were closing and I had to take a 2 hour nap against my will. After the nap I'm still foggy and sleepy. What is going on!!
What did I do wrong? Cauliflower is the only common denominator but that doesn't make sense. The other thing I'm considering is maybe my cortisol is really low in the morning and that's why I have a history of arising late and going to sleep late…So maybe my body can't function before a certain time despite the substantial sleep.
Oh wow, light bulb, cortisol is what determines whether someone is a "morning person" or a "night owl" isn't it.
@Hila yes it does and remember the reset is not linear……
I forgot to mention that I've been losing some weight almost every single day, but today I was a whole 1.5 lbs more than yesterday morning. Also, the feeling of foggy fatigue I had this morning was exactly the feeling I used to get after a lowfat grain breakfast.
Weird.
True… But I want the world now! Haha, thanks for all that you do. CT is next!
This is such a great article that I stumbled upon when looking for some answers.
I don’t know whether you will see this comment but I was wondering whether you could shed some light on what I am experiencing.
I’m a 17 year old male and I recently gained 1.5 stone in 2 months using Cyproheptadine. I weigh 140lbs 5’10” and ever since I finished my regime, I’ve been experiencing a wide range of symptoms that have been getting progressively worse over the past few months. I was experiencing nausea, abnormal sweating, various stretch marks purple, pink and white on waist and buttocks, there are a few white striae on my knees, elbows and very faint vertical white lines on my abdomen that appear and disappear at times and can be raised, I’ve noticed a few horizontal ones on my chest and previous scar tissue has suddenly become bright, these stretch marks make it uncomfortable to sit or lie down.. Last September I experienced Acanthosis Nigricans around my mouth which went away after a few weeks once I started college, it has since come back however it’s been there for a couple of months now and it can be found on my groin area and on the anticubital fossa. On my groin area there is a light brown ring. My nails look as though they are turning translucent and I’m getting a lot of tremors. I was recently having a gastrointestinal problem which I believe was a Candida overgrowth, but which I now believe I have gotten under control/ gotten rid of. In February I had a major petechial outbreak on my feet, I got blood work and everything was normal, a few days later the petechiae went a rusty colour and faded away, since then it came back (not as bad) and it’s since gone again, however I’ve noticed a couple of Spider Angioma’s (just the body) and when I press on them, they refill from the centre. In the past week I’ve been suffering from a mild headache that seems to get worse when lying down, but that has since started to fade away, leaving me feeling heavy headed and a bit woozy. I’ve also been experiencing lots of muscle and eye twitches. CBC/FBC normal, Glucose normal, Thyroid etc negative. I wondering what this is, as it’s impacting my life greatly.
Caspian you need to come on the forum and give a bit more data in the optimal journal part of the forum. Something in your environment seems amiss.
Hi jack. Great article. Late post. One thing that puzzles me about this article is that low cortisol can also come with marked sleeping problems. It is rare to read much about this and it is not explained why this occurs and what to do about it. My cortisol is low, if I take melatonin it seems to reduce it even further and problems get worse. I have been given a lot of bad sleep advice because no one seems to differentiate that treatment needs to differ depending on the cortisol issue.
This is such a great article that I stumbled upon when looking for some answers.
I don’t know whether you will see this comment but I was wondering whether you could shed some light on what I am experiencing.
My answer: I could answer you because your posting link to your nonsense sites. Get real here and then I get answer you.
Very helpful article! I have TBI/PTSD and low cortisol in a.m. and high at night. That sounds like circadian rhythm is off, but with TBI/PTSD and low blood flow to my limbic system, and being a poet, not a scientist, I’d like your thoughts on low cortisol in a.m., low at mid-day and high at night.
I should add – that I have too high 5-HIAA and Serotonin.
Louise read Ubi 22-24 answer is there.
I’m sorry, what is Ubi?
Ubiquitination series on my blog. There are 25 of them
Would the approach to recovery of the adrenals be any different if the HPA axis suppresion is caused by years long usage of topical steroids, now discontinued?
In my opinion yes. Light, solar light at specific times based upon location altitude and population density become critical
I looked up the polupation density studies, interesting, not being discussed elsewhere. I wonder to what extent my current adrenal insufficiency has to do with anti social my whole life.
Also B6 is often mentioned as a go to supplement for both suppressed adrenal function as well as social anxiety, the population density studies may indicate that the mechanism is shared between the two conditions.
If anti social means inside in front a computer…….a ton.
Hi
I’m 36 yearold female who by chance after having kidney stones and needing a ct scan revealed a 3.6 benign tumor on my right adrenal gland!
I have seen 2 different encronigist first one said leave it and keep monitoring it and recently got 2nd opinion and he said take it out.
I don’t have a lot of symptom of cushings I do have pulppatations at times and seen a cardiologist who said I’m fine,I have anxiety at times also irregular periods every 36-45 days and fertility problems.
No hump or weight gain or hair growth but slightly thinning but that’s in the family on my fathers side.i also have insomnia at times especially middle of my cycle!
I’m confused to remove it and scared of what’s to come after surgery.
How can I lower my levels?
Any feedback is appreciated
I’m in Australia
Cheers
Trish
With a tumor it needs treatment, medical of surgical
It’s not true that it’s impossible that carbs at night don’t help people sleep if their liver is working. This is because there is another mechanism that matters: carbs raise insulin, which lower the ratio of BCAAs to tryptophan in the serum, allowing tryptophan to more freely pass through the blood-brain barrier, where it becomes serotonin and then melatonin. Tryptophan supplementation studies have consistently shown decreased sleep latency upon taking tryptophan before bedtime, especially when taken on an empty stomach away from other, competing amino acids.
It is true when those amino acids are missing their hydration shell and the biochemical pathways inside cells are lacking water. the BUN/creat ratio is a proxy for this redox measure. You’ve completely missed that fact and it is critical to get right. Patterns of vibrations are codified in the geometry of shape and size of things that store energy. The most important feature of living things is that they are not heat engines. They do not make their living by heat transfer. The heat liberated by mitochondria is not allowed to enter the environment. It is stored in water because it is a purple and red light chromophore that covers all frequencies in the visible spectrum and passed it into to the optical window of tissues (600nm -1400nm). Sunlight makes our cell water liquid crystalline. Liquid crystalline = coherent water = exclusion zone water. Liquid crystalline water possesses long range orientational order by pointing all the molecules by pointing in the same direction. It also allows for translational order that allows them to keep their position as they move. Liquid crystals are mobile and flexible and highly responsive. This allows them to undergo rapid changes in orientation or phase transitions when energy is added or subtracted from water. This is why cell water responds vigourously to electric or magnetic fields. It is why water responds vigourously to temp, pressure, pH, hydration, and concentrations of inorganic ions like phosphorus. Everything in a cell including lipids and proteins is liquid crystalline because they are hydrated in cell water. The proportion of bound versus free water on the surfaces of lipids and proteins is known to be altered by confirmation changes of the proteins. Water allows the molecular quantum machines inside of cells to work at nearly 100% efficiency because of how water stores sunlight energy. Liquid crystalline water at lipid and protein interfaces provides excitation energy that enables it to split into hydrogen and oxygen in photosynthesis, simultaneously generating food which contains the electric fingerprint in cells. This is the DC electric current Becker found. This liquid crystal is at the heart of all cells because it simultaneously generates electricity in mitochondria by releasing heat into water. This provides for rapid intercommunication between the environment and every living cell. It allows for a massive creation of electrons to be used as a redox pile that drives biochemical reactions because EZ water is excited and it can easily transfer electrons to molecules on its surface. The core chemistry of all life is is the reduction-oxidation or redox potential that transfer electrons between chemical species. This is how biochemistry is designed to be powered by natural sunlight. Water electricity induced by sunlight is special compared to man made electric currents because it also involves the creation of positive charges of protons. Water conducts protons by jumping down a chain of water molecules. This aspect is how enzymes are powered to speed up chemical reactions in biochemistry by a million fold. We have definitive proof now that enzymes do not work if they are not hydrated. This is why dehydatrion is deadly to a far from equillibrium system. When water is confined at scales below 1.6 nm inside of spaces the amount of proton jumping in water explodes. This diameter is where water behaves like it would in a glass capillary tube versus one below 1.4 nm in the opposite way in a temperature diameter phase diagram. This is why people do nit realize water at confinded spaces shrink bigtime at these scales. Not only does nanospace confined water show high temperature superconductivity, it also exhibits superfluidity with flow rates that show enhancement of 50-900 fold that do not fit convential fluid flow theory. The reason is simple: EZ water is a quantum superfuild like helium is at cold temperatures. This is why EZ water around collagen and mitochondria can do things that defy logic. All of the non linear apsects of light are magnified in liquid crystals and limited in solid crystals. Second harmonic generation is huge in liquid crystals but is present but has a limited effect in things like quartz with a solid lattice. The power of second harmonic generation in collagen has been shown to be 100% related to the hydration state of collagen in cells. Biology ignores this. This is why a torn ACL or achilles tendon tell you a lot about the environment a person lives under. The EZ phase changes at the small scales is what powers both enzymes and mitochondria to innovate the living state. Gary Fullerton of Univ of Colorado as proved this in his water models. Delocalized protons freed in water by sunlight allows for very fast jump conduction in EZ water. This is how enzymes and DNA work via proton tunnelling. EZ water has a net negative charge of -100mV to -200mV. This means it also is a perfect DC transformer to make a DC electric current to act as a battery. This is why Wunsch always mentions that any light created on an AC transformer is toxic because it induces dirty electricity and it creates flicker effects which decrease the liquid crystal potential in EZ water. This is what dehydration and a high BUN creatine ratio really are. Cell water powered by sunlight ultimately powers the entire biosphere because of these connections. I think the Universe is powered by water electricity and I believe every cell is powered in the same way. Water is the universal electron and proton donor. When you understand this you begin to see that proton and electron currents in water made by sunlight create currents inside fo cells and over extracellular distances that are capable of delivering physical an chemical messages concerning the redox status of all parts of the cell that are communicated by water networks. This sets in motion the requistie core of chemical reactions that restore the local and global energy balance of all living things.
Studies have proven that a small portion of jasmine rice before bed helps sleep onset. This is because of the surge of Tryptophan the body receives by eating rice. Hence you get an increased level of serotonin (relaxation).
So no, carbs before bed is NOT detrimental to sleep.
You Tamy clearly are clueless about the effect of carbs due to deuterium. Carbs and serotonin increases deuterium to cause massive influx of of deuterium to the CSF. When we see sunrises guess what improves? Sleep does. What does sleep get rid of for us? Deuterium. We sleep to clear deuterium from CSF………watch the video. https://futurism.com/heres-how-sleeping-too-little-literally-transforms-your-brain/
For in depth blogs on the coming age of quantum biology become a Patron and I will teach you and answer your questions direct for the cost of a coffee a month. https://www.patreon.com/DrJackKruse
I have seen you mention before that when you quit taking steroids like prednisone, you should supplement with high doses of D3 and get out in the sunlight early in the morning in order to get your cortisol back to optimal levels. My question is: Why the high doses of D3?
Bump your immune system to nudge it. Wont work if you have bad solar snp’s which is why my members learn about them.
Do you know if there is a connection between adrenal fatigue and chronic sinusitis? It seems like a lot of people with adrenal fatigue have this problem. Could it be because low cortisol equals more inflammation? Or maybe the low cortisol alters the immune system?
Ivy there is.
Could you go a bit more into detail on that? So raising your cortisol can help chronic sinusitis? Maybe a D3 supplement could also help?
Your ASI improves its curves as your connection to the sun and Earth improves. That really is the point of an Adrenal Stress Index. The worse your corticol curve looks in the AM the more likely your sinusitis will destroy you.
I highly suspected something “off” with my cortisol so had it tested recently via salivary home test. My 8am was a bit low. My noon was higher than my 8am. (About 50% higher) Then it trailed off rest of day. Was on a vegan diet for the day, on no meds. Was at home resting all this day. Don’t do caffeine or alcohol. Clean lifestyle. Had hysterectomy last year. Will be 50 in a few weeks.
Can think of no reason why the midday levels would be HIGHER than my first morning level. Can you? Can’t find it discussed anywhere. I’ve had major health challenges (mostly extreme unintentional weight loss, abdominal pain, debilitating fatigue, GI symptoms, etc. Thus my reason for suspecting something systemic such as hypocortisolism. I live in Florida (get plenty of sunshine). Have a stressful but good, meaningful life (mother to 6 kids, all adopted with special needs, including one who is total care/terminal diagnosis). Because I self-ordered this salivary test based on a hunch, now I’m not even sure what to do next. Further testing? Serum cortisol and ACTH stim test next? Other? Appreciate any thoughts you can send my way. Thanks for the article.
I can. Your light hygiene is demolished. I will be doing a podcast with Sherrill Sellmann on this topic to be released soon.